| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website https://jem.elmerpub.com |
Review
Volume 15, Number 3, August 2025, pages 69-80
Craniopharyngiomas, Alterations of Melatonin Secretion and Their Implications: A Systematic Review
Salvatore Gentilea, e , Rossana Ariannaa, Mariarosaria Lavorgnaa, Alice Rodrigueza, Dario Fontanellia, Mario Galieroa, Fiammetta Romanoa, Domenico Serpicoa, Elisabetta Scaranob, Carmine Daliac, Annamaria Colaoa, d, Carolina Di Sommaa, d, e
aEndocrinology Unit, Department of Clinical Medicine and Surgery, University of Naples “Federico II”, Naples, Italy
bUOC Endocrinologia, AORN A. Cardarelli, Naples, Italy
cInternal Medicine, S. Maria Della Pieta Hospital, Nola, Italy
dUNESCO Chair “Education for Health and Sustainable Development”, University of Naples “Federico II”, Naples, Italy
eCorresponding Authors: Carolina Di Somma and Salvatore Gentile, Endocrinology Unit, Department of Clinical Medicine and Surgery, University of Naples “Federico II”, Naples, Italy
Manuscript submitted May 15, 2025, accepted July 5, 2025, published online August 7, 2025
Short title: CPs and Melatonin: A Systematic Review
doi: https://doi.org/10.14740/jem1529
| Abstract | ▴Top |
Craniopharyngiomas are rare sellar tumors that often cause hypothalamic dysfunction due to either their extension or treatment. This dysfunction can disrupt the suprachiasmatic nucleus and impair circadian rhythms like melatonin secretion, with potential effects on sleep, metabolism, and overall quality of life. Despite growing interest, the role of melatoninergic dysregulation in craniopharyngioma survivors remains uncertain. Therefore, this study aims to systematically review the current literature on melatonin secretion in both adult and pediatric craniopharyngioma patients, assess the risk of bias, evaluate the consistency of findings, estimate the certainty of current evidence, and discuss the clinical implications of melatonin alterations. A systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines, using the electronic databases of PubMed/MEDLINE, Embase, Scopus, Web of Science, and the Cochrane Library. The search targeted studies evaluating melatonin secretion in adult and pediatric craniopharyngioma patients, with or without comparisons to healthy controls. The risk of bias was assessed using the Risk of Bias in Non-randomized Studies - of Interventions, Version 2 (ROBINS-I V2) tool, while the overall certainty of evidence was evaluated considering the risk of bias, consistency, directness, precision, and publication bias. Four studies met the inclusion criteria. All reported disrupted melatonin secretion in craniopharyngioma patients, though the patterns varied. Most showed reduced nighttime melatonin levels or altered secretion profiles, particularly regarding release onset and its peak. Significant correlations emerged between melatonin disruption and clinical outcomes such as higher body mass index (BMI), increased daytime sleepiness, poorer sleep quality, reduced physical activity, and altered circadian timing. The risk of bias was low in two studies and moderate to serious in the others, while the overall certainty of evidence was rated as moderate due to the small number of studies and their heterogeneity. Evidence suggests that melatonin secretion is frequently altered in craniopharyngioma survivors, potentially affecting sleep, metabolism, and psychological well-being. While findings are consistent, methodological differences and limited data reduce the certainty of evidence. Future research should prioritize standardized protocols, larger cohorts, and longitudinal designs to clarify the role of melatonin in various comorbidities and the potential of this hormone as both a diagnostic and therapeutic tool. Melatonin may serve not only as a biomarker for hypothalamic injury but also as a possible adjunctive treatment in the context of a hormonal replacement therapy.
Keywords: Craniopharyngioma; Melatonin; Pituitary neoplasm; Hypothalamus; Pineal gland; Circadian rhythm; Hypothalamic disease; Circadian dysfunction
| Introduction | ▴Top |
Craniopharyngiomas (CPs) are rare, locally aggressive neoplasms of the pituitary region originating from embryonic residues of Rathke’s pouch [1]. Their incidence is approximately 0.13 cases per 100,000 person-years, with 30-50% occurring in individuals < 18 years: in this age group, CPs represent 5-11% of intracranial tumors, making them the most common central nervous system (CNS) neoplasm [2-4].
Based on histological features, we classify CPs into two subtypes that differ in microscopy, epidemiology, and molecular characteristics [5].
Adamantinomatous craniopharyngioma (ACP) is predominantly cystic, has a double incidence peak (5 - 15 years and 45 - 60 years), and harbors somatic mutations in CTNNB1, which encodes β-catenin [4, 6].
In contrast, papillary craniopharyngioma (PCP) is usually solid, commonly affects older adults (50 - 60 years), and involves BRAF-V600E mutations [4, 7].
Because they grow along the sellar and suprasellar regions [8], the tumor and its treatment often damage the pituitary axis [9, 10]. This can lead to severe complications, such as panhypopituitarism and hypothalamic disease, which impact quality of life (QoL) and drive various comorbidities, including appetite dysregulation and hypothalamic obesity, thirst dysregulation and diabetes insipidus, body temperature alteration, and sleep disorders [11-13].
Several factors contribute to these manifestations, like hormone deficiencies, altered leptin and hypocretin signaling, and damage to the suprachiasmatic nucleus (SCN), the biological pacemaker regulating circadian rhythms like melatonin secretion and sleep-wake cycles [14-16].
Melatonin, or N-acetyl-5-methoxytryptamine, is a pineal indolamine derived from L-tryptophan [17]. Its complete biochemical synthesis is shown in Figure 1. Historically known for sleep regulation, recent research has stressed its positive effects on oxidative stress, inflammation, metabolism, and cancer [18-20]. Its release strongly depends on light/dark cycle information conveyed from the eye to the SCN by intrinsically photosensitive retinal ganglion cells (ipRGCs) via the retinohypothalamic tract [21-23]. These cells, under dim light conditions, use melanopsin, an excitable photopigment, to photoisomerize the 11-cis-retinal into all-trans-retinal, thereby activating the phospholipase C (PLCB4) pathway and depolarizing [24-26]. The resulting action potential causes the release of glutamate and pituitary adenylate cyclase-activating polypeptide (PACAP), stimulating the SCN neurons to activate the superior cervical ganglia cells of the sympathetic system [27, 28]. At this point, norepinephrine and neuropeptide-Y (NPY) released by their endings induce pinealocytes to increase melatonin levels [29].
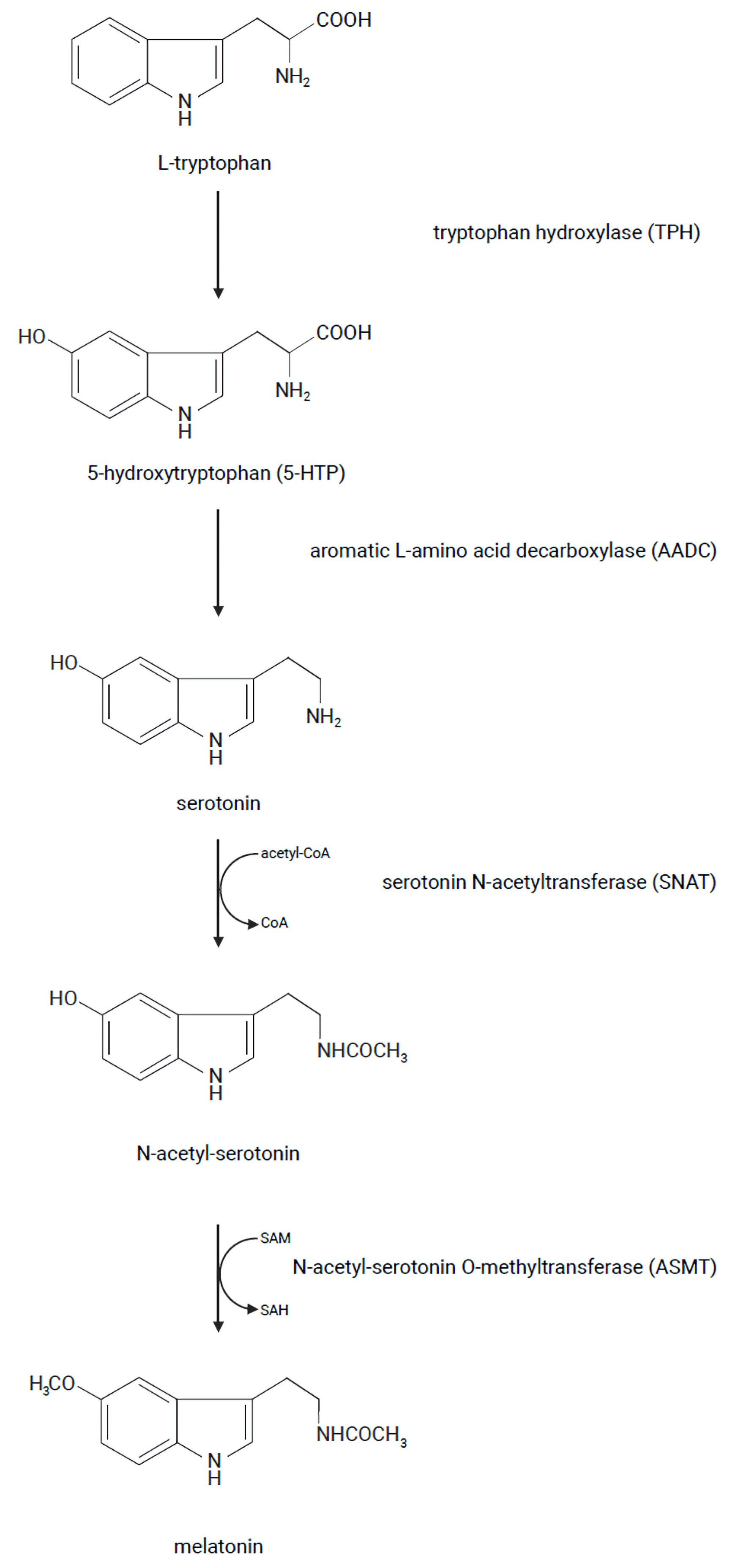 Click for large image | Figure 1. Melatonin synthesis in humans. |
Although several authors point out that hypothalamic damage in CNS tumor survivors alters circadian rhythms [30-32], we lack research focusing on CP patients. Some studies indicate that patients undergoing surgery and/or radiotherapy have a higher prevalence of impaired melatonin release and sleep disorders than the general population [33-37]. However, the findings are inconsistent: while some report reduced melatonin levels, others describe peak irregularities, probably due to methodological heterogeneity. Furthermore, the implications concerning sleep, metabolism, and overall well-being are unclear, as well as melatonin’s role as a relevant biomarker or therapeutic target.
Consequently, this study aims to systematically review the available findings on melatonin secretion in CP patients, focusing on alterations in melatonin levels and their possible implications. Moreover, we want to evaluate the risk of bias and the consistency of results to estimate the certainty of current evidence. Finally, we highlight the need for future studies assessing melatonin as a potential marker and supplement for CP-related hypothalamic disease.
| Materials and Methods | ▴Top |
We formulated a research question using the PICO framework [38], where the population (P) included adult and pediatric patients with CP; the intervention (I) involved the assessment of melatonin secretion patterns; the comparison (C) group consisted of healthy controls; and the outcome (O) focused on alterations in melatonin secretion and their implications.
A systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement and checklist [39]. No language or publication year restrictions were placed to include all relevant studies.
Eligibility criteria
The following inclusion and exclusion criteria were applied to select studies.
Inclusion criteria were: 1) Evaluation of melatonin secretion in CP patients; 2) Involvement of adult or pediatric patients with CP; 3) Validated methods to assess melatonin levels (e.g., plasma, saliva, urine); 4) Full-text articles published in peer-reviewed journals.
Exclusion criteria were: 1) Review articles, editorials, letters, and conference abstracts without sufficient data; 2) Studies not addressing patients with CP; 3) Studies not measuring melatonin secretion; 4) Articles without available full text.
Data sources and search strategy
The following electronic databases were systematically searched between January 17 and 18, 2025: PubMed/MEDLINE, using the query (“Craniopharyngioma” (Mesh) OR craniopharyngioma) AND (“Melatonin” (Mesh) OR melatonin); Embase, with the query (“craniopharyngioma”/exp OR craniopharyngioma) AND (“melatonin”/exp OR melatonin); and Scopus, Web of Science Core Collection, and Cochrane Library using the query “craniopharyngioma” AND “melatonin”.
Duplicate removal
Results from all databases were imported into Zotero for duplicate removal [40].
Selection process
Four reviewers independently selected studies in four steps: 1) Titles and abstracts screening: studies not assessing melatonin secretion in CP patients were excluded; 2) Full-text retrieval: articles were downloaded as PDFs and saved in a desktop folder; 3) Eligibility assessment: studies were assessed based on eligibility criteria, focusing on methods and results; 4) Resolution of discrepancies: disagreements between reviewers were solved through discussion.
Data collection process
The four reviewers collected data independently, each assigned one of the included articles.
Their initials are provided in Table 1 for transparency.
 Click to view | Table 1. Melatonin Secretion Evaluation |
Extracted data included: population characteristics (e.g., age); methods used for melatonin level assessment; melatoninergic system features (e.g., plasma and salivary melatonin levels (pg/mL), dim light melatonin onset (DLMO, clock time)); and associations between melatonin secretion alterations and clinical features, which include: 1) Body mass index (BMI, kg/m2); 2) Sleep/wake cycle characteristics (sleep onset latency (SOL, min), sleep quality (Pittsburgh Sleep Quality Index), total sleep time (min), nighttime sleep duration (min), sleep efficiency (%), and disorders like excessive daytime sleepiness (Epworth Sleepiness Scale (ESS))); 3) Physical activity (activity counts per minute).
Data were entered into an Excel form, and a final collaborative review was conducted to ensure completeness.
Risk of bias assessment
The risk of bias in included studies was evaluated using the Risk of Bias in Non-randomized Studies - of Interventions, Version 2 (ROBINS-I V2) tool [41].
Seven domains were examined: 1) Confounding factors; 2) Classification of interventions; 3) Selection of participants; 4) Deviations from intended interventions; 5) Missing data; 6) Measurement of the outcome; and 7) Selection of the reported result.
Synthesis methods
Given the heterogeneity in methodologies, populations, and outcomes among the studies, a meta-analysis was unfeasible. Instead, the results were synthesized narratively to provide an overview of the key findings.
Figures and tables creation
Microsoft PowerPoint was used to create figures, while Microsoft Word was used to create tables.
Artificial intelligence use
We used ChatGPT (OpenAI, version February 2025, based on the GPT-4) to assist with language refinement and improve the clarity of the manuscript [42]. Specifically, ChatGPT was employed to revise linguistic accuracy and provide suggestions for improving fluency in all sections. The authors verified all scientific content to ensure accuracy and reliability.
| Results | ▴Top |
The search yielded 99 records. After importing them into Zotero for duplicate removal, 24 articles remained.
After screening titles and abstracts,14 records were excluded: four were additional duplicates [43-46] and 10 were irrelevant [47-56]. Next, five studies were excluded because the full text was unavailable [57-61]. Five articles were assessed for eligibility, and one was excluded as it lacked specific data from CP patients [37].
Ultimately, four studies met the criteria for this systematic review [33-36].
The complete PRISMA flowchart of the selection process is presented in Figure 2.
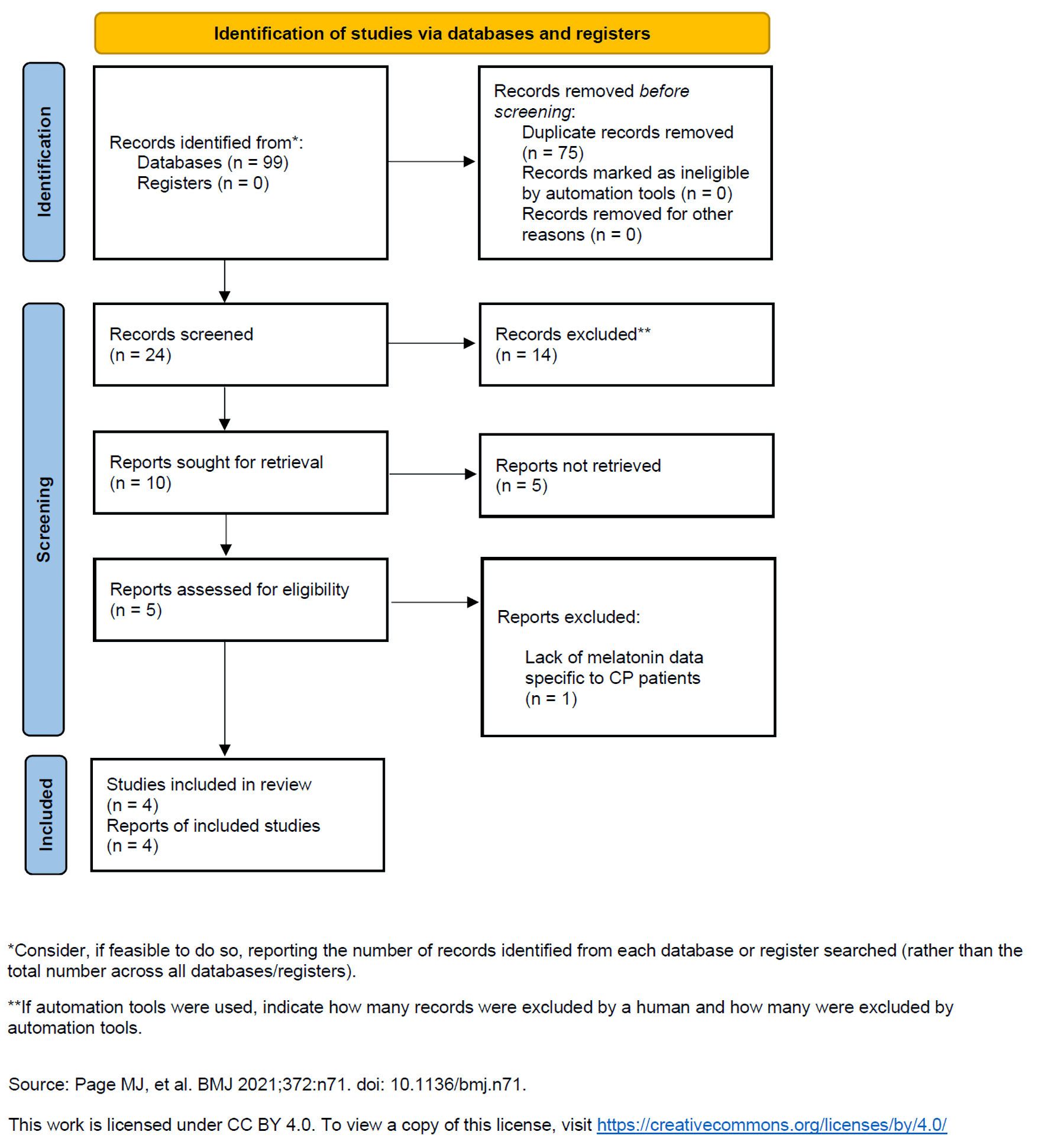 Click for large image | Figure 2. PRISMA flowchart. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses; CP: craniopharyngioma. |
Study characteristics
The included studies vary in their methodologies, populations, and outcomes.
Population
All studies involved patients with CP. Two focused on pediatric patients [34, 36], one included patients aged 18 - 70 [35], and another covered patients aged 6 - 33 [33].
Method of melatonin measurement
Three studies measured salivary melatonin using enzyme-linked immunosorbent assay (ELISA) [36] or radioimmunoassay (RIA) [33, 35], and one assessed plasma melatonin with no specified test [34].
Outcomes
Muller et al [33] examined median salivary melatonin in the morning (6:00 am - 8:00 am), midday (11:00 am - 2:00 pm), evening (6:00 pm - 9:00 pm), and night (11:00 pm - 12:00 am). Lipton’s study [34] evaluated 24-h and nighttime mean plasma melatonin. Pickering’s paper [35] focused on the 24-h median salivary melatonin collecting samples at 12:00 pm, 4:00 pm, 8:00 pm, 10:00 pm, 12:00 am, 4:00 am, 8:00 am, and 12:00 pm. Kamara et al [36] assessed the DLMO, which is the point when melatonin levels rise in response to dim light conditions.
Furthermore, they explored associations between melatonin secretion and clinical features.
Alterations in melatonin levels
The key findings are summarized in Table 1 and described in detail below.
Muller et al [33] found that nighttime salivary melatonin levels were markedly lower in patients with BMI > 4 standard deviation (SD) compared to obese controls (P < 0.0001) but did not significantly differ between non-obese CP patients and healthy controls. Similarly, Lipton’s data [34] show reduced 24-h and nocturnal plasma melatonin compared to historical controls, with an undetectable nighttime peak. Pickering’s research [35] highlights a lower area under the curve (AUC) for salivary melatonin in CP patients than in healthy controls (P = 0.04), indicating reduced secretion.
In conclusion, Kamara et al [36] reported that 47.2% of participants had an invalid DLMO: of these, 19 had elevated initial melatonin levels, two remained below the threshold, and four displayed irregular secretion patterns.
Correlations with clinical variables
Three out of the four studies explored associations between melatonin alterations and clinical features.
Muller et al [33] observed that higher BMI was associated with increased morning melatonin (P = 0.004) and reduced nighttime concentrations (P < 0.001), along with a negative correlation to ESS scores (r: -0.42, P = 0.001 and r: -0.31, P = 0.02, respectively).
Pickering’s study [35] confirmed a negative correlation between midnight melatonin concentrations, ESS scores (r: -0.49, P = 0.08), and sleep quality (r: -0.53, P = 0.06). But, while these two findings did not reach statistical significance, they identified significant associations with reduced total sleep time (r: 0.60, P = 0.03), night sleep duration (r: 0.59, P = 0.03), sleep efficiency (r: 0.62, P = 0.02), and physical activity (r: 0.29, P = 0.04).
In conclusion, Kamara et al [36] highlighted that patients without a measurable DLMO had longer (P = 0.005) and variable (P = 0.043) SOL, while in the subgroup with a valid DLMO, a higher BMI was associated with later onset (r: 0.48, P = 0.012). Furthermore, DLMO timing correlated positively with average waketime (r: 0.40, P = 0.042) and midsleep time (r: 0.47, P = 0.015), and negatively with the standard deviation of SOL (r: -0.47, P = 0.049).
Risk of bias in included studies
The results of the risk of bias assessment are described in detail below and summarized in Table 2.
 Click to view | Table 2. Risk of Bias Assessment |
Bias due to confounding
Muller et al [33] addressed obesity but overlooked other confounders. Lipton et al [34] did not consider potential confounders like BMI or circadian variations. Pickering et al [35] controlled multiple confounders by recruiting gender-, age- and BMI-matched controls and considering hypothalamic injury, hormone insufficiencies, hormone replacement therapies, and sleep characteristics. Kamara et al [36] accounted for melatonin supplementation, hypothalamic involvement, diabetes insipidus, light perception, sleep/wake cycle characteristics, age, sex, BMI, and sleep disorders.
Bias in the classification of exposures
All studies assigned participants to the patients and control groups before the start of the observations based on the presence/absence of CP diagnosis.
Bias in participant selection
Muller et al [33] lacked clear selection criteria. Lipton et al [34] used a small sample size with limited details on the selection process. Pickering et al [35] and Kamara et al [36] defined detailed inclusion and exclusion criteria.
Bias due to deviations from intended interventions
Lipton et al [34] noted one patient lost intravenous access after 40 h instead of the planned 72 h. Muller et al [33], Pickering et al [35], and Kamara et al [36] reported no deviation from the protocol.
Bias due to missing data
Muller et al [33], Pickering et al [35], and Kamara et al [36] excluded non-compliant patients with missing data. Lipton et al [34] recruited only three patients and failed to provide details about one incomplete melatonin data collection.
Bias in the measurement of outcomes
Muller et al [33] and Pickering et al [35] assessed salivary melatonin using RIA; however, while the former did not describe the protocol in detail, the latter provided a comprehensive protocol to reduce bias. Lipton et al [34] collected plasma melatonin samples under dim light conditions (< 10 lux) but did not specify the assay used. Kamara et al [36] instructed caregivers to follow a specific protocol for sample collection and used ELISA for melatonin measurements.
Bias in the selection of reported results
Muller et al [33] reported differences in morning and nighttime melatonin levels but omitted nonsignificant results from comparisons between normal-weight CP patients and controls. Lipton et al [34] did not present polysomnography data, raising concerns about selective reporting. Pickering et al [35] and Kamara et al [36] reported all variables specified in the methods, including both significant and nonsignificant results.
Certainty of evidence for alterations in melatonin secretion in craniopharyngioma patients
Risk of bias
The included studies varied in methodological rigor. While Kamara et al [36] and Pickering et al [35] demonstrated low risks across most domains, Lipton et al [34] presented serious concerns and Muller et al [33] had moderate risk.
Consistency
Results across studies consistently indicate disrupted melatonin secretion in CP patients. However, variations in the type of alteration suggest some heterogeneity.
Directness
All four studies directly addressed melatonin secretion in patients with CP.
Precision
Some factors contribute to uncertainty, such as the small sample size and the use of plasma melatonin evaluations in the study of Lipton et al [34], and the absence of a control group in the study of Kamara et al [36].
Publication bias
There is no clear evidence of publication bias, but we cannot rule it out because of the limited number of studies.
Overall certainty
We rated the certainty of the evidence for alterations in melatonin secretion in CP patients as moderate: while consistent findings support this conclusion, the small number of studies and their heterogeneity lowered the confidence.
| Discussion | ▴Top |
This is the first study to systematically review the relationship between CPs and melatonin production and its clinical implications.
We found that several authors pointed out alterations in the melatonin system in CP survivors, affecting functions like metabolism and sleep. Current evidence does not allow for a definitive distinction between melatonin dysregulation caused directly by the tumor and that resulting from its treatment. However, most studies agree that hypothalamic damage, whether caused by the tumor’s location or by therapeutic interventions such as surgery or radiotherapy affecting the SCN, is the key factor influencing melatonin secretion, by impairing both the afferent and efferent neural pathways responsible for its regulation [15]. Supporting this hypothesis, other studies have described similar pathophysiology for comorbidities like hypothalamic obesity, identifying alterations in the afferent signaling mediated by leptin and in the efferent one linked to α-melanocyte stimulating hormone (α-MSH or melanocortin) [62, 63]. This disruption creates a non-ending vicious cycle of hyperphagia and reduced energy expenditure that leads to excessive weight gain [64, 65].
These findings suggest a link between CP and circadian dysfunction and the consequent hormonal imbalance in the melatoninergic system influences various clinical domains.
First, melatonin dysregulation impacts metabolism and body weight. Muller et al [33] found that CP patients with higher BMI displayed reduced nighttime melatonin and increased daytime one. This finding aligns with other studies linking melatoninergic alterations to metabolic diseases like obesity, diabetes mellitus, and metabolic syndrome [66, 67]. However, the relationship between melatonin and weight gain appears to be bidirectional: while melatonin improves insulin resistance and chronic inflammation, obesity itself associates with chronodisruption, sleep impairment, and melatonin deficiency [68-70]. Melatonin’s ability to inhibit body weight gain is well documented in rodents. For instance, Elliott et al observed that pinealectomized Djungarian hamsters failed to exhibit the typical winter-associated reduction in adiposity [71]. During this season, reduced daylight exposure leads to increased melatonin secretion and a prolonged nocturnal peak, suggesting that melatonin may play a role in promoting fat loss [72]. Supporting this hypothesis, similar findings have been reported in rats. In particular, Wolden-Hanson et al demonstrated that supplementing the drinking water of male rats with melatonin resulted in a significant reduction in body weight, visceral adiposity, leptin, and insulin levels within 2 weeks [73]. In contrast to rodents, evidence regarding the correlation between melatonin levels and metabolic alterations in humans, as well as the potential anti-obesity effects of melatonin supplementation, remains limited. However, a recent study found that in a cohort of 30 adults with metabolic syndrome, the administration of 5 mg of melatonin every evening, 2 h before bedtime, over a 2-month period led to significant improvements in metabolic parameters [74]. Therefore, further clinical trials are warranted, as melatonin supplementation may represent a promising strategy for managing obesity and metabolic syndrome.
Several studies also indicate a relationship between craniopharyngioma and impaired psychological well-being. For example, Memmesheimer et al found that young adults with childhood-onset CP reported reduced psychosocial QoL and increased depression rates, while Mehren et al identified a higher prevalence of apathy among CP patients [75, 76]. These results may be closely linked to hypothalamic and pituitary damage. Indeed, growing evidence suggests that hormone deficiency, such as oxytocin deficiency and hypothalamic obesity contribute to neurobehavioral abnormalities [77-80]. Alongside oxytocin, melatonin likely plays a key role, as circadian dysfunction is strongly associated with psychiatric conditions like major depression, seasonal affective disorder, and bipolar disorder [81-83]. Furthermore, drugs acting on the melatoninergic receptors MT-1 and MT-2, such as agomelatine, have demonstrated efficacy in patients with major depression [84].
Melatonin disruption also profoundly affects the sleep-wake cycle, as evidenced by the studies included in this review, which associate melatonin alterations with poorer sleep quality and a higher prevalence of sleep disorders, such as excessive daytime sleepiness and narcolepsy.
Finally, melatonin might contribute to thermoregulation via several mechanisms, one of which is the induction of the browning of the white adipose tissue [29, 85, 86]. Indeed, Mendes et al found that chronic melatonin supplementation increases the thermogenic potential of aged rats by promoting the conversion of white adipose tissue into beige and brown ones, upregulating uncoupling proteins like UCP1A1 and increasing energy expenditure and heat production [87]. Therefore, melatonin deficiency may be involved in temperature dysregulation like cold intolerance, often observed in CP patients [11, 88-90].
Future research should focus on large-scale, standardized studies to better assess melatonin dysregulation in CP patients and its clinical consequences. We need uniform protocols for melatonin measurement to facilitate data comparability and reliability, as well as longitudinal studies evaluating the long-term impact of altered melatonin secretion on clinical features.
Moreover, few studies have compared melatonin profiles between patients diagnosed in childhood versus adulthood. Considering that the adamantinomatous subtype, which tends to cause more extensive hypothalamic involvement, is more frequent in pediatric cases, a more severe dysregulation of melatonin could be expected in younger patients. Although their study did not focus exclusively on CP but also included other types of sellar neoplasms, Rosenkranz et al did not find any significant differences in the hourly urinary excretion of the melatonin metabolite 6-sulphatoxymelatonin (aMT6s) in relation to the age at disease onset [37].
Furthermore, they did not report any significant group differences in aMT6s excretion based on radiation technique (conformal radiation therapy and gamma knife) and the addition of chemotherapy and/or surgery to radiotherapy [37]. Nonetheless, the study did not explore the individual impact of radiotherapy, chemotherapy, or surgery as separate treatment modalities for CPs.
Future research should therefore also investigate age-related and treatment-related differences in melatonin secretion patterns in CP survivors, in order to better understand how tumor biology and age at diagnosis may influence neuroendocrine outcomes.
Little is known about melatonin’s role as a biomarker. Rosenkranz et al found that there was no significant correlation between hourly urinary excretion of the aMT6s and the presence/absence of pituitary insufficiency [37]. However, their analysis did not stratify patients based on the number of pituitary hormone deficiencies. In contrast, Pickering et al provided a detailed description of the number of affected pituitary axes among participants but did not conduct any test to correlate melatonin levels and the number of hormonal insufficiencies [35]. Thus, new studies should evaluate this correlation to see whether melatonin may be used as a biomarker of the extent of hypothalamic-pituitary damage. Furthermore, the role of melatonin supplementation in CP patients remains uncertain: although Muller et al found that a melatonin daily substitution of 6 mg significantly improved daytime sleepiness and increased physical activity with excellent tolerability, further data are necessary to confirm its benefits and safety [33]. Randomized controlled trials investigating melatonin administration could determine the optimal dosage and clarify its therapeutic potential in this vulnerable population.
Limitations of this study include the small number of articles, their heterogeneity which prevented us from conducting a metanalysis, and the moderate risk of bias which lowers the certainty of evidence and limits the generalizability of our findings. Additionally, studies reporting nonsignificant results may be underrepresented as we cannot rule out publication bias.
On the other hand, key strengths include the systematic, rigorous, and transparent methodology, and the identification of knowledge gaps that future studies should address. This allows for a comprehensive synthesis of current evidence.
In conclusion, this review highlights the significant yet underexplored role of melatonin dysregulation in craniopharyngioma patients. Our findings indicate that these patients have a higher prevalence of melatonin impairment compared to the general population, which seems to impact their QoL. It remains to be determined whether this neurohormone might have a role in diagnostic and therapeutic protocols. Therefore, further studies are needed to confirm these findings and to evaluate the potential of melatonin as a routine biomarker for hypothalamic injury, and its effects when administered as part of a hormonal replacement therapy. A better understanding of melatonin in this context may lead to more holistic strategies to improve the overall QoL of craniopharyngioma survivors.
Acknowledgments
The scientific support of Panta Rei Societa Benefit Srl (https://www.panta-rei.eu/pantarei/, accessed on May 15, 2025) is highly appreciated.
Financial Disclosure
The authors received no financial support for the research, authorship, and publication of this article.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Author Contributions
SG and CDS conceived the study and drafted the manuscript. SG, RA, ML, and AR were responsible for data collection and conducted the systematic review. DF, MG, FR, DS, ES, and CD contributed to the literature search and critically reviewed the paper. CDS and AC supervised the project. All authors contributed to the article and approved the submitted version.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
CPs: craniopharyngiomas; CNS: central nervous system; ACP: adamantinomatous craniopharyngioma; PCP: papillary craniopharyngioma; QoL: quality of life; SCN: suprachiasmatic nucleus; ipRGCs: intrinsically photosensitive retinal ganglion cells; PACAP: pituitary adenylate cyclase-activating polypeptide; NPY: neuropeptide-Y; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses; DLMO: dim light melatonin onset; BMI: body mass index; SOL: sleep onset latency; ESS: Epworth Sleepiness Scale; ROBINS-I V2: Risk of Bias in Non-randomized Studies, of Interventions, Version 2; RIA: radioimmunoassay; ELISA: enzyme-linked immunosorbent assay; SD: standard deviation; AUC: area under the curve; α-MSH: α-melanocyte stimulating hormone; aMT6s: 6-sulphatoxymelatonin
| References | ▴Top |
- Joynt RJ. Clinical Neurology. 1998. Ch14. p. 50.
- Karavitaki N, Cudlip S, Adams CB, Wass JA. Craniopharyngiomas. Endocr Rev. 2006;27(4):371-397.
doi pubmed - Bunin GR, Surawicz TS, Witman PA, Preston-Martin S, Davis F, Bruner JM. The descriptive epidemiology of craniopharyngioma. J Neurosurg. 1998;89(4):547-551.
doi pubmed - Rosemberg S, Fujiwara D. Epidemiology of pediatric tumors of the nervous system according to the WHO 2000 classification: a report of 1,195 cases from a single institution. Childs Nerv Syst. 2005;21(11):940-944.
doi pubmed - Apps JR, Muller HL, Hankinson TC, Yock TI, Martinez-Barbera JP. Contemporary Biological Insights and Clinical Management of Craniopharyngioma. Endocr Rev. 2023;44(3):518-538.
doi pubmed - Hara T, Akutsu H, Takano S, Kino H, Ishikawa E, Tanaka S, Miyamoto H, et al. Clinical and biological significance of adamantinomatous craniopharyngioma with CTNNB1 mutation. J Neurosurg. 2019;131(1):217-226.
doi pubmed - Brastianos PK, Taylor-Weiner A, Manley PE, Jones RT, Dias-Santagata D, Thorner AR, Lawrence MS, et al. Exome sequencing identifies BRAF mutations in papillary craniopharyngiomas. Nat Genet. 2014;46(2):161-165.
doi pubmed - Gao Q, Luo J, Pan J, Zhang L, Song D, Zhang M, Xu D, et al. Integrative analyses identify HIF-1alpha as a potential protective role with immune cell infiltration in adamantinomatous craniopharyngioma. Front Immunol. 2022;13:949509.
doi pubmed - van Schaik J, Hoving EW, Muller HL, van Santen HM. Hypothalamic-pituitary outcome after treatment for childhood craniopharyngioma. Front Horm Res. 2021;54:47-57.
doi pubmed - Donson AM, Apps J, Griesinger AM, Amani V, Witt DA, Anderson RCE, Niazi TN, et al. Molecular analyses reveal inflammatory mediators in the solid component and cyst fluid of human adamantinomatous craniopharyngioma. J Neuropathol Exp Neurol. 2017;76(9):779-788.
doi pubmed - Thompson CJ, Costello RW, Crowley RK. Management of hypothalamic disease in patients with craniopharyngioma. Clin Endocrinol (Oxf). 2019;90(4):506-516.
doi pubmed - Castle-Kirszbaum M, Shi MDY, Goldschlager T. Quality of life in craniopharyngioma: a systematic review. World Neurosurg. 2022;164:424-435.e422.
doi pubmed - Romigi A, Feola T, Cappellano S, De Angelis M, Pio G, Caccamo M, Testa F, et al. Sleep Disorders in Patients With Craniopharyngioma: A Physiopathological and Practical Update. Front Neurol. 2021;12:817257.
doi pubmed - Iyigun I, Alikasifoglu A, Gonc N, Ozon A, Eryilmaz Polat S, Hizal M, Kiper N, et al. Obstructive sleep apnea in children with hypothalamic obesity: Evaluation of possible related factors. Pediatr Pulmonol. 2020;55(12):3532-3540.
doi pubmed - Cordani R, Veneruso M, Napoli F, Di Iorgi N, Milanaccio C, Consales A, Disma N, et al. Sleep disturbances in pediatric craniopharyngioma: a systematic review. Front Neurol. 2022;13:876011.
doi pubmed - Amaral FGD, Cipolla-Neto J. A brief review about melatonin, a pineal hormone. Arch Endocrinol Metab. 2018;62(4):472-479.
doi pubmed - Zhang JJ, Meng X, Li Y, Zhou Y, Xu DP, Li S, Li HB. Effects of melatonin on liver injuries and diseases. Int J Mol Sci. 2017;18(4):673.
doi pubmed - Cajochen C, Krauchi K, Wirz-Justice A. Role of melatonin in the regulation of human circadian rhythms and sleep. J Neuroendocrinol. 2003;15(4):432-437.
doi pubmed - Imenshahidi M, Karimi G, Hosseinzadeh H. Effects of melatonin on cardiovascular risk factors and metabolic syndrome: a comprehensive review. Naunyn Schmiedebergs Arch Pharmacol. 2020;393(4):521-536.
doi pubmed - Calastretti A, Gatti G, Lucini V, Dugnani S, Canti G, Scaglione F, Bevilacqua A. Melatonin analogue antiproliferative and cytotoxic effects on human prostate cancer cells. Int J Mol Sci. 2018;19(5):1505.
doi pubmed - Cardinali DP, Pevet P. Basic aspects of melatonin action. Sleep Med Rev. 1998;2(3):175-190.
doi pubmed - Brennan R, Jan JE, Lyons CJ. Light, dark, and melatonin: emerging evidence for the importance of melatonin in ocular physiology. Eye (Lond). 2007;21(7):901-908.
doi pubmed - Weng SJ, Sheng WL, Gong X, Yang XL, Zhong YM. Modulatory effects of melatonin on intrinsically photosensitive retinal ganglion cells in the rat. Invest Ophthalmol Vis Sci. 2017;58(8):4138.
- Berson DM, Dunn FA, Takao M. Phototransduction by retinal ganglion cells that set the circadian clock. Science. 2002;295(5557):1070-1073.
doi pubmed - Graham DM, Wong KY. Melanopsin-expressing, Intrinsically Photosensitive Retinal Ganglion Cells (ipRGCs). In: Kolb H, Fernandez E, Jones B, Nelson R, eds. Webvision: The Organization of the Retina and Visual System. Salt Lake City (UT). 1995.
pubmed - Xue T, Do MT, Riccio A, Jiang Z, Hsieh J, Wang HC, Merbs SL, et al. Melanopsin signalling in mammalian iris and retina. Nature. 2011;479(7371):67-73.
doi pubmed - Hannibal J, Hindersson P, Knudsen SM, Georg B, Fahrenkrug J. The photopigment melanopsin is exclusively present in pituitary adenylate cyclase-activating polypeptide-containing retinal ganglion cells of the retinohypothalamic tract. J Neurosci. 2002;22(1):RC191.
doi pubmed - Moller M, Baeres FM. The anatomy and innervation of the mammalian pineal gland. Cell Tissue Res. 2002;309(1):139-150.
doi pubmed - Claustrat B, Leston J. Melatonin: Physiological effects in humans. Neurochirurgie. 2015;61(2-3):77-84.
doi pubmed - Slawik H, Stoffel M, Riedl L, Vesely Z, Behr M, Lehmberg J, Pohl C, et al. Prospective study on salivary evening melatonin and sleep before and after pinealectomy in humans. J Biol Rhythms. 2016;31(1):82-93.
doi pubmed - Datta A, Das KK, G KK, Jaiswal AK, Kumar R. Temporal profile of serum melatonin levels in paediatric pineal tumours subjected to surgery: newer insights. Childs Nerv Syst. 2023;39(9):2285-2292.
doi pubmed - Murata J, Sawamura Y, Ikeda J, Hashimoto S, Honma K. Twenty-four hour rhythm of melatonin in patients with a history of pineal and/or hypothalamo-neurohypophyseal germinoma. J Pineal Res. 1998;25(3):159-166.
doi pubmed - Muller HL, Handwerker G, Gebhardt U, Faldum A, Emser A, Kolb R, Sorensen N. Melatonin treatment in obese patients with childhood craniopharyngioma and increased daytime sleepiness. Cancer Causes Control. 2006;17(4):583-589.
doi pubmed - Lipton J, Megerian JT, Kothare SV, Cho YJ, Shanahan T, Chart H, Ferber R, et al. Melatonin deficiency and disrupted circadian rhythms in pediatric survivors of craniopharyngioma. Neurology. 2009;73(4):323-325.
doi pubmed - Pickering L, Jennum P, Gammeltoft S, Poulsgaard L, Feldt-Rasmussen U, Klose M. Sleep-wake and melatonin pattern in craniopharyngioma patients. Eur J Endocrinol. 2014;170(6):873-884.
doi pubmed - Kamara D, Crowley SJ, Crabtree VM, Hancock D, Li Y, Darji H, Semko J, et al. Circadian rhythms in pediatric craniopharyngioma. Front Sleep. 2023;2:1153144.
doi - Rosenkranz E, Thissen A, Siegel S, Piroth M, Clusmann H, Gebauer J, Brabant G, et al. Melatonin secretion following brain midline irradiation is diminished, but not correlated with subjective sleep disturbances. Clin Endocrinol (Oxf). 2018;89(6):870-877.
doi pubmed - Richardson WS, Wilson MC, Nishikawa J, Hayward RS. The well-built clinical question: a key to evidence-based decisions. ACP J Club. 1995;123(3):A12-13.
pubmed - Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
doi pubmed - Roy Rosenzweig Center for History and New Media. Zotero [Computer software]. George Mason University. 2025. Retrieved from: https://www.zotero.org/.
- Sterne JAC, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, Henry D, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;355:i4919.
doi - OpenAI. ChatGPT (February 2025 version). Language model based on GPT-4. 2025. Retrieved from: https://www.openai.com/.
- 2009 Late-Breaking Science Abstracts. Neurology 73, fasc. 4. 2009. https://www.embase.com/search/results?subaction=viewrecord&id=L70007415&from=export.
- Kamara D, Crabtree VM, Crowley S, Hancock D, Semko J, Merchant T, Mandrell e B. Circadian rhythms among youth with craniopharyngioma. Sleep. 2022;45(suppl 1):A280.
doi - Ilyina E, Strebkova N, Peterkova e V. Melatonin deficiency and disrupted circadian rhythms in pediatric survivors of craniopharyngioma. Hormone Research in Paediatrics. 2012;78:230.
doi - Jakobsen LP, Klose M, Gammeltoft S, Jennum P, Feldt-Rasmussen e U. Sleep-wake pattern and its association with melatonin, as a marker of the circadian function of the suprachiasmatic nucleus. Craniopharyngioma Patients. Endocrine Reviews. 2013;34(3). https://www.embase.com/search/results?subaction=viewrecord&id=L71784627&from=export.
- Verberne LM, Maurice-Stam H, Grootenhuis MA, Van Santen HM, Schouten-Van Meeteren AY. Sleep disorders in children after treatment for a CNS tumour. J Sleep Res. 2012;21(4):461-469.
doi pubmed - van Schaik J, Pillen S, van Litsenburg RRL, Vandenbussche NLE, de Bont JM, Schouten-van Meeteren AYN, van Santen HM. The importance of specialized sleep investigations in children with a suprasellar tumor. Pituitary. 2020;23(6):613-621.
doi pubmed - Pickering L, Klose M, Feldt-Rasmussen U, Jennum P. Polysomnographic findings in craniopharyngioma patients. Sleep Breath. 2017;21(4):975-982.
doi pubmed - Romijn JA. Pituitary diseases and sleep disorders. Curr Opin Endocrinol Diabetes Obes. 2016;23(4):345-351.
doi pubmed - Manley PE, McKendrick K, McGillicudy M, Chi SN, Kieran MW, Cohen LE, Kothare S, et al. Sleep dysfunction in long term survivors of craniopharyngioma. J Neurooncol. 2012;108(3):543-549.
doi pubmed - Joustra SD, Kruijssen E, Verstegen MJ, Pereira AM, Biermasz NR. Determinants of altered sleep-wake rhythmicity in patients treated for nonfunctioning pituitary macroadenomas. J Clin Endocrinol Metab. 2014;99(12):4497-4505.
doi pubmed - de Almeida EA, Di Mascio P, Harumi T, Spence DW, Moscovitch A, Hardeland R, Cardinali DP, et al. Measurement of melatonin in body fluids: standards, protocols and procedures. Childs Nerv Syst. 2011;27(6):879-891.
doi pubmed - Josephine A, Aulinas A. Physiology of the pineal gland and melatonin. In: Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, et al. Endotext. South Dartmouth (MA): MDText.com, Inc., 2000.
- Cordani R, Veneruso M, Napoli F, Di Iorgi N, Milanaccio C, Consales A, Disma N, et al. Sleep disturbances in craniopharyngioma: a challenging diagnosis. A case series and review of the literature. Journal of Sleep Research. 2022;31:e13740.
doi - Cordani R, Veneruso M, Napoli F, Milanaccio C, Verrico A, Consales A, Cataldi M, et al. Sleep disturbances in craniopharyngioma: a challenging diagnosis. Sleep Medicine. 2022;100:S104-S105.
doi - LaRosa KN, Crowley SJ, Hancock D, Caples M, Merchant TE, Crabtree VM, Mandrell B. Assessment of sleep-wake and circadian rhythm disruption in children and adolescents diagnosed with craniopharyngioma. Sleep. 2020;43(SUPPL 1):A377-A378.
doi - Jennum P, Frahm-Falkenberg S, Knudsen S. Secondary narcolepsy - case presentation and evaluation. Journal of Sleep Research. 2012;21:51.
doi - Frahm-Falkenberg S, Knudsen S, Gammeltoft S, Jennum P. Hypothalamic craniopharyngeoma resulting in hypocretin deficiency and narcolepsy with atypical cataplexy. European Journal of Neurology. 2011;18:334.
doi - Baranowska B, Soszynski P, Misiorowski W. Circadian melatonin rhythm in women with hypothalamic amenorrhoea. Neuroendocrinology Letters. 1986;8(6):295-300.
- Muller HL, Handwerker G, Wollny B, Faldum A, Sorensen N. Melatonin secretion and increased daytime sleepiness in childhood craniopharyngioma patients. J Clin Endocrinol Metab. 2002;87(8):3993-3996.
doi pubmed - Iughetti L, Bruzzi P. Obesity and craniopharyngioma. Ital J Pediatr. 2011;37:38.
doi pubmed - Roth CL, McCormack SE. Acquired hypothalamic obesity: A clinical overview and update. Diabetes Obes Metab. 2024;26(Suppl 2):34-45.
doi pubmed - van Santen HM, Denzer C, Muller HL. Could setmelanotide be the game-changer for acquired hypothalamic obesity? Front Endocrinol (Lausanne). 2023;14:1307889.
doi pubmed - Daousi C, Dunn AJ, Foy PM, MacFarlane IA, Pinkney JH. Endocrine and neuroanatomic features associated with weight gain and obesity in adult patients with hypothalamic damage. Am J Med. 2005;118(1):45-50.
doi pubmed - Szewczyk-Golec K, Wozniak A, Reiter RJ. Inter-relationships of the chronobiotic, melatonin, with leptin and adiponectin: implications for obesity. J Pineal Res. 2015;59(3):277-291.
doi pubmed - Ramirez AVG, Filho DR, de Sa L. Melatonin and its relationships with diabetes and obesity: a literature review. Curr Diabetes Rev. 2021;17(7):e072620184137.
doi pubmed - Guan Q, Wang Z, Cao J, Dong Y, Chen Y. Mechanisms of melatonin in obesity: a review. Int J Mol Sci. 2021;23(1):218.
doi pubmed - Prado NJ, Ferder L, Manucha W, Diez ER. Anti-inflammatory effects of melatonin in obesity and hypertension. Curr Hypertens Rep. 2018;20(5):45.
doi pubmed - Reiter RJ, Tan DX, Korkmaz A, Ma S. Obesity and metabolic syndrome: association with chronodisruption, sleep deprivation, and melatonin suppression. Ann Med. 2012;44(6):564-577.
doi pubmed - Elliott JA, Bartness TJ, Goldman BD. Effect of melatonin infusion duration and frequency on gonad, lipid, and body mass in pinealectomized male Siberian hamsters. J Biol Rhythms. 1989;4(4):439-455.
doi pubmed - Bartness TJ, Wade GN. Photoperiodic control of seasonal body weight cycles in hamsters. Neurosci Biobehav Rev. 1985;9(4):599-612.
doi pubmed - Wolden-Hanson T, Mitton DR, McCants RL, Yellon SM, Wilkinson CW, Matsumoto AM, Rasmussen DD. Daily melatonin administration to middle-aged male rats suppresses body weight, intraabdominal adiposity, and plasma leptin and insulin independent of food intake and total body fat. Endocrinology. 2000;141(2):487-497.
doi pubmed - Kozirog M, Poliwczak AR, Duchnowicz P, Koter-Michalak M, Sikora J, Broncel M. Melatonin treatment improves blood pressure, lipid profile, and parameters of oxidative stress in patients with metabolic syndrome. J Pineal Res. 2011;50(3):261-266.
doi pubmed - Memmesheimer RM, Lange K, Dolle M, Heger S, Mueller I. Psychological well-being and independent living of young adults with childhood-onset craniopharyngioma. Dev Med Child Neurol. 2017;59(8):829-836.
doi pubmed - Mehren A, Ozyurt J, Zu Klampen P, Boekhoff S, Thiel CM, Muller HL. Self- and informant-rated apathy in patients with childhood-onset craniopharyngioma. J Neurooncol. 2018;140(1):27-35.
doi pubmed - Mann A, Kalitsi J, Jani K, Martins D, Kapoor RR, Paloyelis Y. The oxytocin system in patients with craniopharyngioma: A systematic review. Front Neuroendocrinol. 2025;76:101170.
doi pubmed - Brandi ML, Gebert D, Kopczak A, Auer MK, Schilbach L. Oxytocin release deficit and social cognition in craniopharyngioma patients. J Neuroendocrinol. 2020;32(5):e12842.
doi pubmed - Clarke L, Zyga O, Pineo-Cavanaugh PL, Jeng M, Fischbein NJ, Partap S, Katznelson L, et al. Socio-behavioral dysfunction in disorders of hypothalamic-pituitary involvement: The potential role of disease-induced oxytocin and vasopressin signaling deficits. Neurosci Biobehav Rev. 2022;140:104770.
doi pubmed - Ozyurt J, Mehren A, Boekhoff S, Muller HL, Thiel CM. Social cognition in patients with hypothalamic-pituitary tumors. Front Oncol. 2020;10:1014.
doi pubmed - Quera Salva MA, Hartley S, Barbot F, Alvarez JC, Lofaso F, Guilleminault C. Circadian rhythms, melatonin and depression. Curr Pharm Des. 2011;17(15):1459-1470.
doi pubmed - Satyanarayanan SK, Su H, Lin YW, Su KP. Circadian rhythm and melatonin in the treatment of depression. Curr Pharm Des. 2018;24(22):2549-2555.
doi pubmed - Dedmari T, Ramzan S, Hussain Masoodi M, Hassan Mir R. Detailed review of melatonin and its role in managing the symptoms of depression. Curr Mol Med. 2025.
doi pubmed - Cardinali DP, Srinivasan V, Brzezinski A, Brown GM. Melatonin and its analogs in insomnia and depression. J Pineal Res. 2012;52(4):365-375.
doi pubmed - Kuthati Y, Lin SH, Chen IJ, Wong CS. Melatonin and their analogs as a potential use in the management of Neuropathic pain. J Formos Med Assoc. 2019;118(8):1177-1186.
doi pubmed - Machado SA, Pasquarelli-do-Nascimento G, da Silva DS, Farias GR, de Oliveira Santos I, Baptista LB, Magalhaes KG. Browning of the white adipose tissue regulation: new insights into nutritional and metabolic relevance in health and diseases. Nutr Metab (Lond). 2022;19(1):61.
doi pubmed - Mendes C, Gomes G, Belpiede LT, do Carmo Buonfiglio D, Motta-Teixeira LC, Amaral FG, Cipolla-Neto J. The effects of melatonin daily supplementation to aged rats on the ability to withstand cold, thermoregulation and body weight. Life Sci. 2021;265:118769.
doi pubmed - Hiramatsu K, Takahashi K, Ikeda A, Arimori S. A case of intrasellar craniopharyngioma. Tokai J Exp Clin Med. 1987;12(2):135-140.
pubmed - Lamas Oliveira C. Metabolic consequences of craniopharyingioma and their management. Endocrinol Nutr. 2013;60(9):529-534.
doi pubmed - Clar HE. Disturbances of the hypothalamic thermoregulation. Acta Neurochir (Wien). 1985;75(1-4):106-112.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.