| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website https://jem.elmerpub.com |
Original Article
Volume 15, Number 5, December 2025, pages 191-201
Impact of Disease-Specific Counseling on Quality of Life and Glycemic Control in Different Types of Diabetes
Nishant Jaina, Sourav Debnathb, g, Mahaveer Singha, g, Dogga Sudhakara, Nidhi Sharmac, Prashant Jaind, Sumit Rajotiyab, Sunil Kumar Gurjara, Abhishek Guptae, Anurag Kumar Singhb, Shivang Mishrab, Deepak Nathiyab, Balvir Singh Tomarf
aDepartment of Endocrinology, National Institute of Medical Sciences and Research, Nims University Rajasthan, Jaipur 303121, India
bDepartment of Pharmacy Practice, National Institute of Medical Sciences and Research, Nims University Rajasthan, Jaipur 303121, India
cDepartment of Pathology, National Institute of Medical Sciences and Research, Nims University Rajasthan, Jaipur 303121, India
dTresor Systems Private Limited, Okhla Phase II, New Delhi 110020, India
eDepartment of Medical Gastroenterology, National Institute of Medical Sciences and Research, Nims University Rajasthan, Jaipur 303121, India
fInstitute of Pediatric Gastroenterology and Hepatology, National Institute of Medical Sciences and Research, Nims University Rajasthan, Jaipur 303121, India
gCorresponding Authors: Sourav Debnath, Department of Pharmacy Practice, National Institute of Medical Sciences and Research, Nims University Rajasthan, Jaipur 303121, India; Mahaveer Singh, Department of Endocrinology, National Institute of Medical Sciences and Research, Nims University Rajasthan, Jaipur 303121, India
Manuscript submitted September 11, 2025, accepted November 12, 2025, published online December 24, 2025
Short title: Impact of Counseling in Diabetes
doi: https://doi.org/10.14740/jem1563
| Abstract | ▴Top |
Background: Diabetes mellitus (DM) is associated with metabolic complications and impaired health-related quality of life (HRQoL). While pharmacological therapy remains central to management, structured counseling may provide additional benefits. This study evaluated the impact of counseling on glycemic control and HRQoL among individuals with type 1 diabetes mellitus (T1DM), type 2 diabetes mellitus (T2DM), and pancreatic DM.
Methods: This prospective interventional study included 150 adults with diabetes (T1DM: 30%, T2DM: 54%, pancreatic DM: 16%). Baseline assessments comprised glycemic parameters and HRQoL, measured using the Short Form-36 Health Survey (SF-36) questionnaire. Participants received individualized counseling on diet, exercise, medication adherence, and self-care, with follow-up assessments after 3 months.
Results: Significant improvements were observed in glycemic control and HRQoL. Mean glycated hemoglobin (HbA1c) decreased from 11.06±2.15% to 10.52±2.55% (P = 0.002), and random blood sugar declined from 303.9 ± 29.8 mg/dL to 263.3 ± 60.5 mg/dL (P < 0.001). The SF-36 Physical Component Score improved from 37.4 ± 12.8 to 39.4 ± 13.3 (P < 0.001), and the SF-36 Mental Component Score increased from 29.1 ± 13.3 to 33.1 ± 12.7 (P < 0.001). The greatest improvements were observed in T2DM, whereas pancreatic DM patients showed comparatively modest gains.
Conclusions: Structured, disease-specific counseling significantly enhanced both glycemic control and SF-36-derived HRQoL scores. These findings emphasize the importance of integrating counseling interventions into routine, patient-centered diabetes care.
Keywords: Diabetes mellitus; Glycemic control; Health-related quality of life; Patient counseling; Lifestyle intervention; Self-care adherence
| Introduction | ▴Top |
Diabetes mellitus (DM) is a chronic metabolic disorder that has emerged as a major global health concern. In 2024, an estimated 589 million adults between 20 and 79 years of age were living with the condition, and projections suggest that this number will reach 852.5 million by 2050, marking a steep rise over the next quarter century [1]. The distribution of diabetes is uneven across populations. Men outnumber women by nearly 9.8 million cases [1], and urban areas report almost twice the burden compared to rural settings, with prevalence rates of 12.7% and 8.8%, respectively [1]. Regional differences are also striking, with the Middle East and North Africa recording the highest prevalence at 32.3% and Africa the lowest at 7.8% [1]. India alone accounts for 89.8 million individuals with diabetes, ranking second only to China, and the prevalence is expected to increase by more than 75% by 2050 [1].
The disease is characterized by persistent hyperglycemia, which contributes to long-term complications affecting multiple organ systems. However, the impact of diabetes extends beyond physical health. It often disrupts emotional well-being, causes fatigue, reduces physical functioning, and limits social participation [2]. Common symptoms such as excessive thirst, frequent urination, and weight changes add to this psychosocial burden [3].
Quality of life is a broad and multidimensional concept that reflects how individuals perceive their physical health, mental state, independence, personal growth, and social relationships [4-7]. It offers a holistic measure of well-being, emphasizing that health is not defined solely by the absence of disease but also by the ability to live productively and meaningfully [8, 9].
Although pharmacological therapy is essential for glycemic control, non-pharmacological strategies are increasingly recognized as equally vital. Disease-specific counseling is one such approach that has gained attention for its dual benefit of improving metabolic outcomes and enhancing quality of life [10]. Counseling typically includes individualized advice on diet, physical activity, medication adherence, self-monitoring, and coping strategies. Evidence from clinical trials and meta-analyses highlights that structured counseling significantly reduces glycated hemoglobin (HbA1c) levels, strengthens self-management skills, and leads to better patient-reported outcomes in individuals with type 2 diabetes mellitus (T2DM) [11, 12].
Despite this evidence, counseling is rarely integrated into routine practice in many public healthcare settings in India. Heavy patient loads, limited consultation time, and scarcity of trained personnel often prevent its systematic implementation [13]. Furthermore, most previous research has evaluated the effects of counseling interventions primarily in patients with T2DM, with comparatively little focus on type 1 diabetes mellitus (T1DM) and pancreatic diabetes. These forms differ substantially in their clinical and psychosocial profile. T1DM requires lifelong insulin therapy and education on hypoglycemia prevention; T2DM emphasizes lifestyle modification, weight management, and oral medication adherence; whereas pancreatic diabetes (type 3c) involves both insulin and enzyme replacement due to combined endocrine and exocrine dysfunction [14]. Given these distinctions, counseling strategies must be adapted to address the unique metabolic and psychosocial challenges faced by each group.
With these gaps in mind, the present study was designed to evaluate the role of structured, disease-specific counseling in improving both glycemic control and health-related quality of life (HRQoL) among individuals with T1DM, T2DM, and pancreatic diabetes. We proposed that targeted counseling interventions would result in measurable improvements in glycemic parameters and quality of life scores over a 3-month period.
| Materials and Methods | ▴Top |
Study setting and population
This prospective, interventional study was conducted between October 2024 and April 2025 under the aegis of the National Institute of Medical Sciences and Research, NIMS University, Jaipur, Rajasthan, India.
Ethical approval was obtained from the Institutional Ethics Committee (IEC) of NIMS University (approval No. NIMSUR/IEC/2024/1312). All participants provided written informed consent after being briefed on the study’s objectives, procedures, and confidentiality safeguards.
The study adhered strictly to the ethical guidelines of the Indian Council of Medical Research (ICMR) and the principles outlined in the Declaration of Helsinki (1975). Reporting followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines to ensure methodological rigor and transparency.
Study population
The study population comprised 150 adult patients aged 18 years and above who attended the regular endocrinology outpatient clinic or were referred during inpatient admission at NIMS Hospital, Jaipur, Rajasthan.
Eligibility criteria
Adults aged 18 years and above with a confirmed diagnosis of T1DM, T2DM, or pancreatic diabetes were considered eligible for the study, provided they gave informed consent and agreed to comply with follow-up requirements. Pancreatic diabetes was defined as diabetes secondary to chronic pancreatitis or pancreatic resection, commonly referred to as type 3c DM.
Individuals were excluded if they had gestational DM, were critically ill, or had significant mental incapacity that hindered participation. Patients already enrolled in structured diabetes education programs were also excluded. Additional exclusion criteria included the presence of major systemic comorbidities such as chronic kidney disease, chronic liver disease, malignancy, prolonged intensive care unit stay, rheumatoid arthritis, connective tissue disorders, or severe cognitive impairment. Patients with concurrent major endocrine disorders such as thyroid dysfunction, adrenal disease, or autoimmune polyendocrine syndromes were also excluded from participation.
Sample size
The required sample size was calculated using Cochran’s formula (n = z2 × p × q/e2), where z is the z-score for the desired confidence level, p is the estimated population proportion, q = 1 - p, and e is the margin of error. Using a 95% confidence interval (z = 1.96), a population proportion of 10% (p = 0.10, q = 0.90), and a margin of error of 5% (e = 0.05), the minimum required sample size was calculated to be 139. To account for a potential 5-10% loss to follow-up and incomplete responses, the final sample size was rounded to 150 participants.
Sampling technique
Participants were recruited using a simple random sampling method. A computer-generated list of random numbers was prepared, and patients corresponding to these numbers were selected from the diabetes clinic registry. This approach ensured that every eligible participant had an equal chance of selection and allowed equitable representation across various socioeconomic and geographic groups.
Covariates
Sociodemographic variables
The sociodemographic variables collected included age (in years), age category (< 20 years, 21 - 35 years, 36 - 50 years, 51 - 65 years, > 65 years), gender (male/female), area of living (rural/urban) and marital status (married, unmarried, widow/widower).
Lifestyle variables
Information on lifestyle habits was obtained directly from the patients’ information sheet and verified through a structured questionnaire. Participants were asked about their current use of alcohol, smoking, and smokeless tobacco products. Smoking referred to the use of combustible tobacco products such as cigarettes or bidis, while tobacco intake referred to the use of smokeless forms such as chewing tobacco, gutkha, or khaini. Responses were recorded as “yes” or “no” based on current use at the time of enrollment. For analysis, only participants who reported current use (yes) were considered as positive for the respective variable.
Clinical parameters
Type of diabetes (T1DM, T2DM, or pancreatic DM), duration of diabetes (in months), and diabetes-related symptoms including polyuria, polydipsia, polyphagia, weight loss, anorexia, malaise, and shortness of breath were assessed. Information on these symptoms was obtained using a structured symptom checklist, recorded as present or absent based on patient self-report and verified from clinical records. Systolic and diastolic blood pressure were measured in mm Hg using a standardized digital sphygmomanometer after at least 15 min of rest in the seated position.
Anthropometric variables
Height (m), weight (kg), and body mass index (BMI) - calculated as weight (kg) divided by height squared (m2) -were recorded and classified using Asian-Pacific cut-offs: underweight (< 18.5 kg/m2), normal (18.5 - 22.9 kg/m2), overweight (23 - 24.9 kg/m2), obese class I (25 - 29.9 kg/m2), and obese class II (> 30 kg/m2) [15].
Tools used for assessment
The study evaluated participants’ HRQoL using Short Form-36 (HRQoL-SF-36) score (a validated tool comprising 36 questions that assess physical and mental health components [16, 17]). The results provide two key scores: Physical Component Summary (PCS) and Mental Component Summary (MCS). Each score ranges from 0 to 100, with higher scores indicating better HRQoL. Participants self-administered the questionnaire at baseline to track HRQoL status. The SF-36 is known for its reliability and simplicity and has been extensively used in both clinical and population studies. This score was administered at baseline and at 3 months’ follow-up.
Intervention: disease-specific counseling
The Information-Motivation-Behavioral (IMB) model formed the theoretical basis for the counseling intervention, emphasizing that accurate information, motivation, and behavioral skills collectively drive sustained health behavior change. Patients attending the endocrinology outpatient department or referred during inpatient admission were enrolled in the study. Disease-specific counseling was conducted by a team from the Department of Endocrinology and trained diabetes educators. The counseling framework was standardized across all participants according to the IMB model. However, specific emphasis areas were tailored according to the type of diabetes. Patients with T1DM received additional focus on insulin adherence and prevention of hypoglycemia. Those with T2DM were guided primarily on lifestyle modification and adherence to oral medications. Participants with pancreatic diabetes were counseled regarding nutritional management and the importance of pancreatic enzyme supplementation.
Each participant attended a single structured in-person counseling session lasting approximately 30 - 45 min, followed by fortnightly telephonic reinforcement sessions over 3 months. The counseling included education on diabetes, its complications, and the importance of glycemic control; individualized dietary counseling based on glycemic goals and comorbidities; structured exercise recommendations; medication adherence support; and stress and symptom management. Sessions were supported with printed handouts, PowerPoint presentations, demonstrations, and interactive discussions. Participants were reassessed at the end of the 3-month follow-up period.
Statistical analysis
Data normality was assessed using the Kolmogorov-Smirnov test to determine the appropriate statistical tests for continuous variables. Descriptive statistics were used to summarize the characteristics of the study population, with continuous variables presented as means and standard deviations (SD) and categorical variables as frequencies and percentages. Group comparisons were conducted based on quality of life and glycemic control. Independent t-tests were used for normally distributed continuous variables, while Mann-Whitney U tests were employed for non-normally distributed data. Chi-square tests were used to compare categorical variables. Paired t-tests or Wilcoxon signed-rank tests were applied for pre- and post-intervention comparisons, and analysis of variance (ANOVA) or Kruskal-Wallis tests were used for comparisons between diabetes subgroups. Statistical significance was set at P < 0.05. All analyses were performed using IBM SPSS software version 29.
| Results | ▴Top |
Baseline characteristics
A total of 150 participants were enrolled, with T2DM comprising the majority (54.0%), followed by T1DM (30.0%) and pancreatic DM (16.0%). The mean age of participants was 42.56 ± 15.00 years, with T2DM patients significantly older (52.01 ± 11.87 years) than T1DM (27.11 ± 7.27 years) (P < 0.001). Most participants were male (62.0%) and from rural areas (54.0%). Significant differences were observed across diabetes types in BMI (P < 0.001), with a higher proportion of underweight individuals in the T1DM group. The median duration since diabetes diagnosis was longest in individuals with T1DM (66 months; interquartile range (IQR): 24 - 108), followed by T2DM (48 months; IQR: 36 - 72) and pancreatic diabetes (31 months; IQR: 15 - 48) (P = 0.001) (Table 1).
 Click to view | Table 1. Baseline Sociodemographic of the Study Participants (N = 150) |
Clinical presentation
Polyuria was the most common presenting symptom overall (82.7%) and was significantly more frequent among individuals with pancreatic diabetes (100%, P = 0.021). Weight loss (100%, P = 0.002) and anorexia (75%, P = 0.005) were also markedly more prevalent in the pancreatic diabetes group. In contrast, among the type 1 and type 2 diabetes groups, the distribution of presenting symptoms such as polyuria, polydipsia, polyphagia, malaise, anorexia, and shortness of breath was comparable, with no statistically significant differences observed between them (P > 0.05) (Supplementary Material 1, jem.elmerpub.com).
Baseline physical and laboratory investigations
Systolic blood pressure is higher in individuals with type 1 diabetes (128.90 ± 13.10 mm Hg). Similarly, diastolic blood pressure is also higher in type 1 diabetes (80.69 ± 8.87 mm Hg) as compared to T2DM patients. Hemoglobin (Hb) levels were significantly lower in T2DM patients (12.16 ± 0.83 g/dL vs. 12.58 ± 1.04 g/dL in T1DM, P < 0.001). Significant differences were also noted in high-density lipoprotein cholesterol (HDL-C), triglycerides, liver enzymes (alanine aminotransferase (ALT) and aspartate aminotransferase (AST)) and albumin levels across groups (P < 0.05) (Supplementary Material 2, jem.elmerpub.com).
Impact of disease-specific counseling on HRQoL and glycemic outcomes
Table 2 shows that individualized counseling on diet, exercise, and medication significantly improved all HRQoL domains (P < 0.001). Physical Component Score increased from 37.4 to 39.4 (P < 0.01), and Mental Component Score from 29.1 to 33.1 (P < 0.01), reflecting enhanced overall well-being (Fig. 1).
 Click to view | Table 2. Impact of Disease-Specific Counseling on HRQoL Domains (N = 150) |
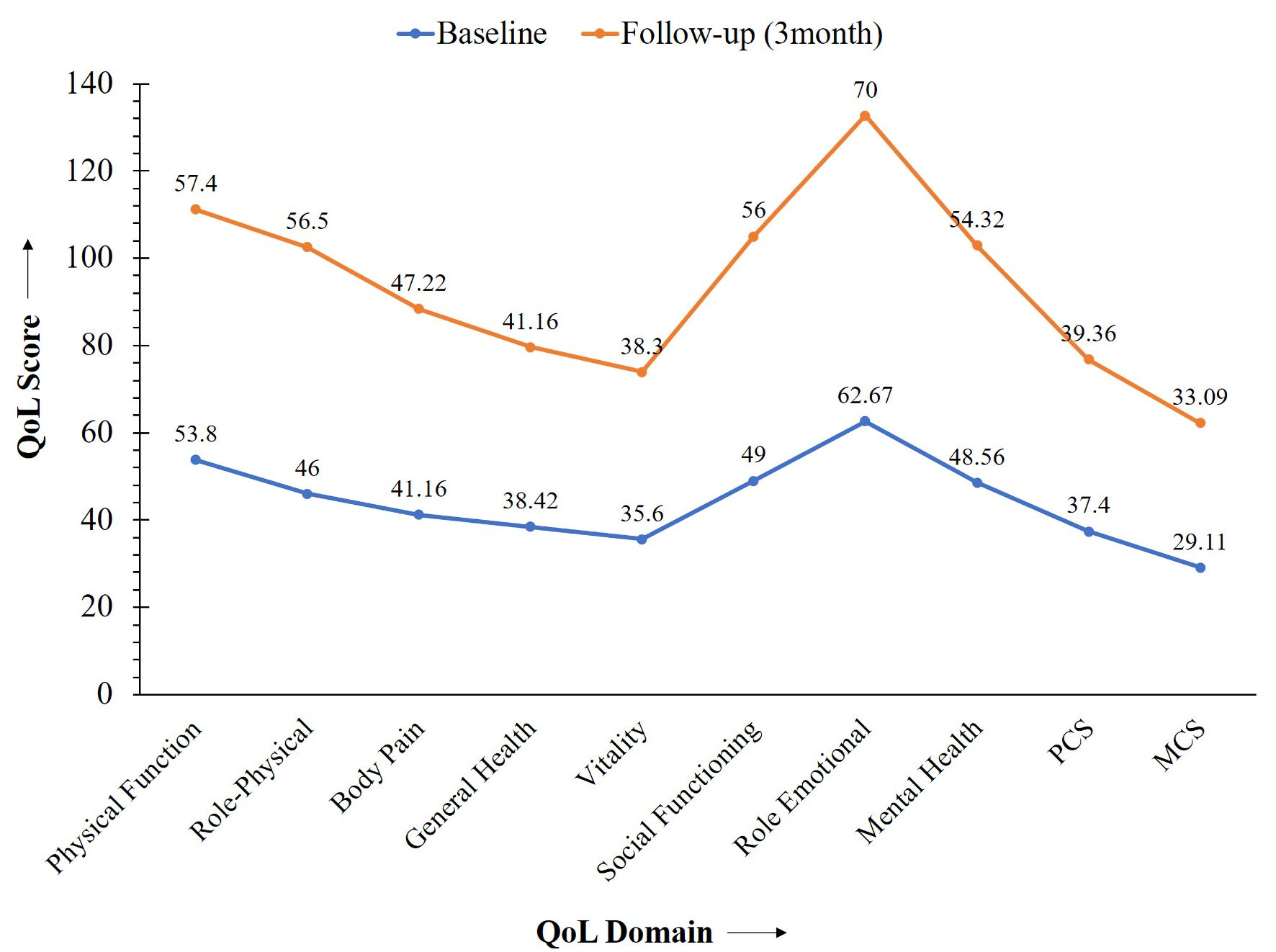 Click for large image | Figure 1. Impact of structural counseling on glycemic control. HRQoL: health-related quality of life; PCS: Physical Component Score; MCS: Mental Component Score. |
At baseline, pancreatic diabetes patients reported the poorest HRQoL, with markedly lower physical functioning (35.0 ± 20.1), general health (18.4 ± 12.2), vitality (19.4 ± 16.8), and mental health (37.5 ± 9.6), compared with type 1 diabetes (physical functioning 67.3 ± 26.7; general health 45.3 ± 31.2; vitality 44.7 ± 30.5; mental health 55.5 ± 24.3) and type 2 diabetes (physical functioning 51.9 ± 31.4; general health 40.6 ± 25.2; vitality 35.4 ± 24.1; mental health 48.0 ± 18.3) (all P < 0.01). Composite scores were also lowest in pancreatic diabetes (PCS 31.5 ± 9.8 vs. 39.5 ± 13.3 in T1DM and 38.0 ± 12.9 in T2DM, P = 0.038) (Table 3).
 Click to view | Table 3. Baseline HRQoL Across Different Types of Diabetes (N = 150) |
After 3 months, improvements were noted in all groups, though pancreatic diabetes remained disadvantaged. Physical functioning rose modestly to 40.0 ± 15.7, compared with 68.0 ± 27.1 in T1DM and 56.7 ± 30.9 in T2DM (P = 0.001). Mental health improved but stayed lowest in pancreatic diabetes (42.5 ± 12.3 vs. 62.9 ± 17.9 in T1DM, P < 0.001). PCS and MCS remained significantly lower in this group (Table 4).
 Click to view | Table 4. HRQoL at Three Months Across Different Types of Diabetes (N = 150) |
Glycemic analysis showed that baseline HbA1c was highest in pancreatic diabetes (12.35 ± 1.1) compared with T1DM (11.07 ± 2.2) and T2DM (10.67 ± 2.2) (P = 0.003). After 3 months, HbA1c showed significant improvement in T1DM (11.07 ± 2.2 to 10.76 ± 2.1, P = 0.042) and T2DM (10.67 ± 2.2 to 9.93 ± 2.8, P = 0.031), whereas the reduction in pancreatic diabetes (12.35 ± 1.1 to 12.05 ± 1.4) was minimal and not statistically significant (P = 0.184). Although the absolute change appeared numerically similar in T1DM and pancreatic diabetes, only the T1DM group demonstrated a statistically significant decline due to greater within-group variability. Random blood sugar also declined significantly in T1DM and T2DM, with minimal change in pancreatic diabetes (P = 0.004) (Table 5). Overall glycemic control improved notably over the 3-month follow-up. Mean HbA1c reduced by 0.54% (from 11.06% to 10.52%, P = 0.002), while random blood sugar showed a 13.4% decrease (from 303.85 mg/dL to 263.27 mg/dL, P < 0.001) (Fig. 2).
 Click to view | Table 5. Glycemic Variability at Baseline and Three Months Across Different Types of Diabetes (N = 150) |
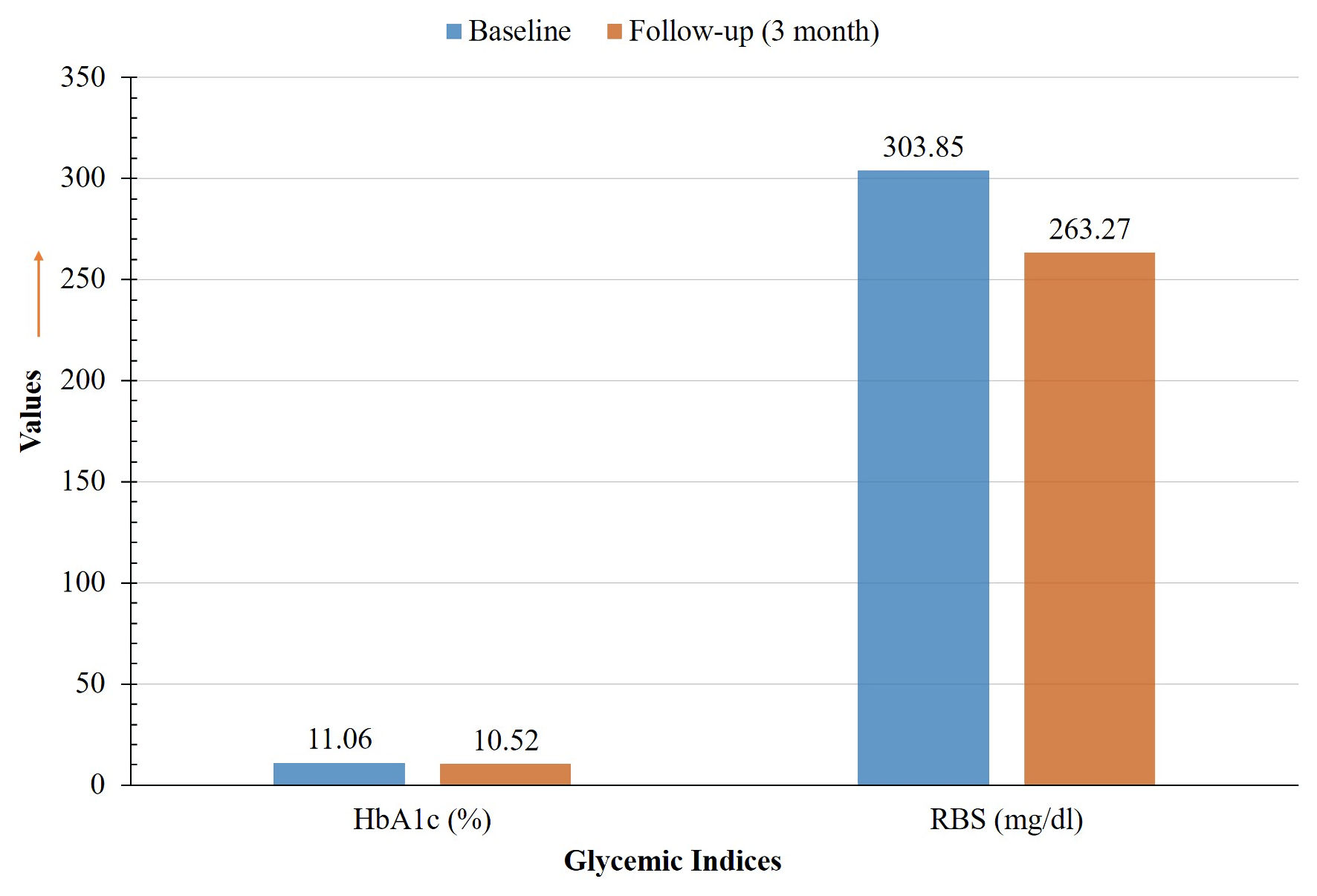 Click for large image | Figure 2. Impact of disease-specific counseling on HRQoL domains. HbA1c: glycated hemoglobin; RBS: random blood sugar. |
| Discussion | ▴Top |
This study evaluated the impact of structured, disease-specific counseling on glycemic control and HRQoL in patients with T1DM, T2DM, and pancreatic diabetes. The findings demonstrate that individualized counseling interventions can produce significant improvements in both glycemic parameters and HRQoL over a 3-month period.
Our results align with existing evidence highlighting the critical role of nutritional education in improving glycemic outcomes in T2DM [18]. Patients who adhered to these individualized dietary recommendations achieved greater reductions in HbA1c, supporting the idea that enhanced nutritional awareness fosters healthier eating patterns and better metabolic control. The role of physical activity is similarly well established. A randomized controlled trial in Japan reported that structured exercise significantly improved glycemic regulation [19], and evidence from South India confirmed better outcomes in patients adhering to dietary and pharmacological regimens [20]. Our findings corroborate these observations, as patients receiving individualized counseling on diet, physical activity, and medication adherence achieved meaningful improvements in glycemic control.
Participant demographics in our study further illustrate the heterogeneity of diabetes in real-world settings. The mean age was 42.56 ± 15.00 years, which is younger than the 53.4 ± 10.3 years reported in another Indian cohort [21]. This difference likely reflects the inclusion of younger T1DM patients. In addition, the T1DM group included a higher proportion of underweight individuals, while pancreatic diabetes patients presented with a greater symptom burden, including polyuria, anorexia, and weight loss. The increased symptom load in pancreatic diabetes likely stems from multifactorial causes, such as concomitant exocrine insufficiency, nutritional malabsorption, and impaired counter-regulatory hormone balance due to deficient insulin and glucagon secretion. Chronic inflammation and recurrent abdominal pain associated with pancreatitis may further exacerbate fatigue and poor appetite, collectively diminishing physical functioning and quality of life [22, 23]. These findings highlight the clinical variability across diabetes subtypes and reinforce the importance of tailoring counseling approaches to the unique pathophysiological and psychosocial needs of each group.
In terms of glycemic outcomes, HbA1c decreased from 11.06% to 10.52%, representing an absolute reduction of 0.54%. Random blood sugar fell from 303.85 mg/dL to 263.27 mg/dL, corresponding to a 13.37% reduction. Although clinically meaningful, these improvements were smaller than those reported in other studies. For example, a randomized trial in India observed a 1.3% reduction in HbA1c following a structured diabetes self-management education (DSME) program [21]; and a Saudi Arabian study reported an even greater decrease of 1.74±0.28% [24]. Several factors may explain the relatively modest reductions observed in our study. First, unlike studies that focused exclusively on T2DM, our cohort included T1DM and pancreatic diabetes patients, who often require intensive insulin therapy and may be less responsive to educational interventions alone. Second, baseline HbA1c values in our population were markedly higher, reflecting poorer initial control and making large reductions more difficult within a short timeframe. Third, although counseling was structured and reinforced through fortnightly follow-ups, the 3-month intervention period was shorter than in some studies that used more frequent or multimodal strategies, such as weekly sessions or group-based education. Finally, socioeconomic barriers and limited healthcare access, particularly among rural participants, likely restricted adherence and reduced the overall impact of the intervention.
Despite these challenges, significant improvements in HRQoL were observed across all domains of the SF-36 assessment. The Physical Component Score improved from 37.40 to 39.36, while the Mental Component Score increased from 29.11 to 33.09. These findings are consistent with a Tunisian study, where DSME enhanced both metabolic outcomes and quality of life in children and adolescents with T1DM [25]. A community-based DSME program in the United States also demonstrated improvements in mental health among patients with T2DM, further emphasizing the psychosocial benefits of structured education [26].
The broader literature reinforces these results. A systematic review confirmed that DSME produces significant improvements in glycemic control and psychosocial well-being, particularly in T2DM patients [27]. A study from China demonstrated that structured self-monitoring of blood glucose improved both metabolic outcomes and quality of life in patients with poorly controlled diabetes, regardless of insulin use [28]. An Indian randomized trial using culturally adapted DSME modules also reported reductions in diabetes-related distress and improved metabolic outcomes [21].
Nevertheless, patients with pancreatic diabetes remained disadvantaged despite counseling. Their glycemic indices improved only minimally, and HRQoL scores for physical functioning and vitality remained low, even though some domains such as role emotional showed improvement. These findings are consistent with the complex pathophysiology of type 3c diabetes, which involves a combination of endocrine and exocrine insufficiency, malnutrition, and postoperative sequelae [29]. Literature consistently notes that outcomes and quality of life in this group are influenced by factors such as chronic pain, malabsorption, and surgical history, and that counseling alone is insufficient. Multidisciplinary care that includes nutritional support, enzyme replacement, and psychological interventions is required to address the specific needs of this subgroup.
The variation in outcomes observed between our cohort and reports from more resource-rich settings may largely reflect socioeconomic and healthcare accessibility differences. In resource-limited populations, constraints such as reduced access to endocrinologists, inconsistent medication supply, and limited diabetes education services often compromise both glycemic control and quality of life [30]. Lower literacy levels, economic stress, and sociocultural factors may further hinder adherence to lifestyle and pharmacological recommendations. In contrast, structured care models with multidisciplinary diabetes teams and sustained counseling support, commonly available in higher income populations, facilitate better self-management and long-term metabolic stability. These disparities emphasize the importance of strengthening community-based diabetes education and ensuring equitable access to healthcare infrastructure in low- and middle-income regions, such as India, particularly in the post-pandemic era, where global disruptions have further widened health inequities [31].
Taken together, our study adds to the growing body of evidence supporting structured, personalized, and context-specific educational strategies in diabetes management. Although the glycemic improvements were modest, the consistent enhancements in HRQoL highlight the multidimensional value of disease-specific counseling, particularly in diverse and resource-limited populations.
Limitations and strengths
This study has certain limitations that warrant consideration. First, the study was uncontrolled and lacked a comparator group, which limits the ability to attribute observed improvements solely to the intervention. Second, the relatively short intervention period of 3 months may not fully reflect the long-term impact of disease-specific counseling on glycemic outcomes. Third, adherence to dietary, physical activity, and medication advice was primarily self-reported, raising the possibility of recall or reporting bias. Incorporating objective adherence measures would have strengthened the reliability of the findings. Fourth, although the counseling was structured, delivery variations and reliance on fortnightly telephonic follow-up may have reduced the intervention’s intensity compared with more comprehensive education models that include frequent in-person sessions or digital group-based support. Fifth, the inclusion of patients with T1DM, T2DM, and pancreatic diabetes introduced clinical heterogeneity. While this design reflects real-world practice, it may have diluted effect sizes for specific subgroups. Finally, the predominantly rural composition of our cohort may limit generalizability, and socioeconomic barriers could have constrained patients’ ability to adopt and sustain recommended behaviors.
Despite these limitations, the study offers important strengths. It is among the few to assess counseling effects across three major diabetes subtypes, providing a broad perspective on educational interventions. Even brief and low-cost counseling yielded meaningful improvements in glycemic control and HRQoL, underscoring the multidimensional benefits of structured education. Although diabetes-related distress was not specifically measured, it is an important factor influencing self-care and outcomes; future studies should include standardized assessments to address this aspect. The pragmatic design in a resource-limited setting also highlights the scalability and real-world relevance of such interventions.
Conclusions
This study demonstrates that structured, disease-specific counseling can significantly improve both glycemic control and quality of life in patients with T1DM, T2DM, and pancreatic diabetes, even within the constraints of rural Indian healthcare settings. Although challenges such as limited resources, restricted healthcare access, and clinical heterogeneity were present, the results underscore the importance of personalized educational strategies in diabetes care. The findings suggest that integrating low-cost, scalable counseling into routine clinical practice can enhance not only metabolic outcomes but also psychosocial well-being. Such approaches hold particular promise for underserved populations, offering a practical and sustainable model for strengthening diabetes management in resource-constrained environments.
| Supplementary Material | ▴Top |
Suppl 1. Baseline clinical presentation of study participants (n = 150).
Suppl 2. Baseline physical and laboratory parameters of study participants (n = 150).
Acknowledgments
The authors express their sincere gratitude to NIMS University for prompt administrative support. Special thanks are extended to the Departments of Pathology and Biochemistry for their valuable assistance in laboratory investigations, and to the Department of Endocrinology for their continuous guidance and support throughout the study.
Financial Disclosure
No source of external funding was applied in this study.
Conflict of Interest
No conflict of interest relevant to this article was reported.
Informed Consent
Written informed consent was obtained from all participants prior to enrollment in the study.
Author Contributions
Conceptualization: NJ and SD; methodology: NJ and MS; software: AG; validation: MS and AKS; formal analysis: PJ and SR; investigation: NS and DS; resources: SKG; data curation: AKS and SM; writing - original draft preparation: NJ and SD; writing - review and editing: MS; visualization: PJ; supervision: MS and BST; project administration: DN; funding acquisition: BST.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
DM: diabetes mellitus; T1DM: type 1 diabetes mellitus; T2DM: type 2 diabetes mellitus; HRQoL: health-related quality of life; SF-36: Short Form-36 Health Survey; HbA1c: glycated hemoglobin; RBS: random blood sugar; PCS: Physical Component Score; MCS: Mental Component Score; DSME: diabetes self-management education; BMI: body mass index; CI: confidence interval; IEC: Institutional Ethics Committee
| References | ▴Top |
- International Diabetes Federation. IDF Diabetes Atlas, 11th ed. Brussels, Belgium: 2025.
- Trikkalinou A, Papazafiropoulou AK, Melidonis A. Type 2 diabetes and quality of life. World J Diabetes. 2017;8(4):120-129.
doi pubmed - Nicolucci A, Kovacs Burns K, Holt RI, Comaschi M, Hermanns N, Ishii H, Kokoszka A, et al. Diabetes Attitudes, Wishes and Needs second study (DAWN2): cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabet Med. 2013;30(7):767-777.
doi pubmed - Abolfathi M, Pasdar Y, Kheiri M, Irandoost SF, Darabi F. The effect of consuming multivitamin/mineral supplements on elderly quality of life: Based on randomized control trial. J Educ Health Promot. 2021;10:63.
doi pubmed - Liu J, Wang S, Leng J, Li J, Huo X, Han L, Liu J, et al. Impacts of gestational diabetes on quality of life in Chinese pregnant women in urban Tianjin, China. Prim Care Diabetes. 2020;14(5):425-430.
doi pubmed - Solhi M, Irandoost SF, Abolfathi M. Investigating the status of quality of life of drivers of freight trucks of the city of Kermanshah and the factors influencing it, Iran Occup. Health J. 2021;18:231-242.
- Zhianfar L, Solhi M, Azar FEF, Hosseini AF, Irandoost SF. The effect of educational intervention based on social support theory on improvement of hemodialysis patients’ quality of life. Iranian Journal of Health, Saf Environ. 2021;7:1473-1477.
- Marquesin NA, Lima SA, Costa RA, Rodrigues MR, Ferraz GA, Molina AC, Cassetari BF, et al. Health related quality of life in pregnant women with diabetes or mild hyperglycemia. Int Arch Med. 2016;9.
- Zokaei A, Ziapour A, Khanghahi ME, Lebni JY, Irandoost SF, Toghroli R, Mehedi N, et al. Investigating high blood pressure, type-2 diabetes, dislipidemia, and body mass index to determine the health status of people over 30 years. J Educ Health Promot. 2020;9:333.
doi pubmed - Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013;12(1):14.
doi pubmed - Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ Couns. 2016;99(6):926-943.
doi pubmed - Powers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, Hess-Fischl A, Hooks B, et al. Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Educ. 2020;46(4):350-369.
doi pubmed - Joshi R, Alim M, Kengne AP, Jan S, Maulik PK, Peiris D, Patel AA. Task shifting for non-communicable disease management in low and middle income countries—a systematic review. PLoS One. 2014;9(8):e103754.
doi pubmed - American Diabetes Association Professional Practice Committee. 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes-2025. Diabetes Care. 2025;48(Suppl 1):1 S181-S206.
doi pubmed - Lim JU, Lee JH, Kim JS, Hwang YI, Kim TH, Lim SY, Yoo KH, et al. Comparison of World Health Organization and Asia-Pacific body mass index classifications in COPD patients. Int J Chron Obstruct Pulmon Dis. 2017;12:2465-2475.
doi pubmed - Ware JE, Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473-483.
pubmed - McHorney CA, Ware JE, Jr., Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247-263.
doi pubmed - Gebreyesus HA, Abreha GF, Besherae SD, Abera MA, Weldegerima AH, Kidane EG, Bezabih AM, et al. Eating behavior among persons with type 2 diabetes mellitus in North Ethiopia: a cross-sectional study. BMC Endocr Disord. 2021;21(1):99.
doi pubmed - Terauchi Y, Takada T, Yoshida S. A randomized controlled trial of a structured program combining aerobic and resistance exercise for adults with type 2 diabetes in Japan. Diabetol Int. 2022;13(1):75-84.
doi pubmed - Durai V, Samya V, Akila GV, Shriraam V, Jasmine A, Muthuthandavan AR, Gayathri T, et al. Self-care practices and factors influencing self-care among type 2 diabetes mellitus patients in a rural health center in South India. J Educ Health Promot. 2021;10:151.
doi pubmed - Anjali M, Khapre M, Kant R, Kumar S, Pandey P. Effectiveness of diabetes self-management education on distress and HbA1C among Indian type 2 diabetes mellitus patients: a randomized controlled trial. Indian J Community Med. 2023;48(5):702-708.
doi pubmed - Ewald N, Bretzel RG. Diabetes mellitus secondary to pancreatic diseases (Type 3c)—are we neglecting an important disease? Eur J Intern Med. 2013;24(3):203-206.
doi pubmed - ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, et al. 2. Classification and diagnosis of diabetes: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S19-S40.
doi pubmed - Almotairy KA, Sabbagh TT, Alkhuli MA, Tallab MA, Hawsawi RA, Baroom NA. The impact of health education on hemoglobin A1C in diabetic patients at the family medicine department of king fahad armed forces hospital in Jeddah. Cureus. 2024;16(12):e75627.
doi pubmed - Bouslama A, et al. Effect of diabetes self-management education on HRQoL in Tunisian children with T1DM and their parents: A randomized controlled trial.
- Sugiyama T, Steers WN, Wenger NS, Duru OK, Mangione CM. Effect of a community-based diabetes self-management empowerment program on mental health-related quality of life: a causal mediation analysis from a randomized controlled trial. BMC Health Serv Res. 2015;15:115.
doi pubmed - Kicaj E, Saliaj A, Cercizaj R, Prifti V, Qirko S, Rogozea L. Navigating diabetes: enhancing self-management through education among diabetic people at the early stages of the disease-a systematic review. Int J Environ Res Public Health. 2024;21(5):522.
doi pubmed - Kan K, Zhu W, Lu F, Shen Y, Gao F, Mo Y, He X, et al. Contribution of structured self-monitoring of blood glucose to the glycemic control and the quality of life in both insulin- and noninsulin-treated patients with poorly controlled diabetes. Diabetes Technol Ther. 2017;19(12):707-714.
doi pubmed - Wayne CD, Benbetka C, Besner GE, Narayanan S. Challenges of Managing Type 3c Diabetes in the context of pancreatic resection, cancer and trauma. J Clin Med. 2024;13(10).
doi pubmed - Lall D, Engel N, Devadasan N, Horstman K, Criel B. Challenges in primary care for diabetes and hypertension: an observational study of the Kolar district in rural India. BMC Health Serv Res. 2019;19(1):44.
doi pubmed - Magliano DJ, Boyko EJ, Atlas ID. COVID-19 and diabetes. InIDF Diabetes Atlas [Internet]. 10th edition. 2021. International Diabetes Federation.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.